

Oncology Learning Collaborative Partnership
Only 14% of cancers are detected through preventive screening, with most cancers discovered through physician visits that include physical exams, along with in-depth discussions about signs and symptoms. The reduction in screening rates due to the pandemic still lingers and is worrisome.
Underlying the support for screening and early identification is the fact that survival rates increase through early detection. There is a financial motivation, too. Late-stage cancer treatment typically costs significantly more than early-stage cancer treatment, and late-stage treatment takes a larger human toll in stress and side effects.

Screening and Early Identification
One of the project’s goals is to connect cancer prevention, early identification, and all the other ways to improve cancer outcomes. Many employers are concerned about low cancer screening rates, especially since they have not rebounded post-pandemic, as expected. Delays in screenings delay diagnosis of cancer and subsequent treatment which increases the risk of poor outcomes and higher costs of care.
Patients may not be aware of recommended cancer screenings:
- The American Cancer Society recommends that people at average risk of colorectal cancer start regular screening at age 45. This can be done either with a sensitive test that looks for signs of cancer in a person’s stool (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam).
- The United States Preventive Services Task Force now recommends that all women get screened for breast cancer every other year.
- AHIP and a coalition of public and private health organizations launched in June 2024 “Promoting Health through Prevention,” a coordinated campaign to publicize the availability of preventive services for no out-of-pocket cost under the Affordable Care Act. The coalition will use several tools and services to educate Americans about the importance of preventive services, including the use of MyHealthfinder.
Outreach to individuals who have missed recommended screenings can be undertaken by the carrier and/or a patient’s primary care provider. Employers are encouraged to ask carriers how they conduct outreach and what the success rate is for plan members catching up on recommended screenings.
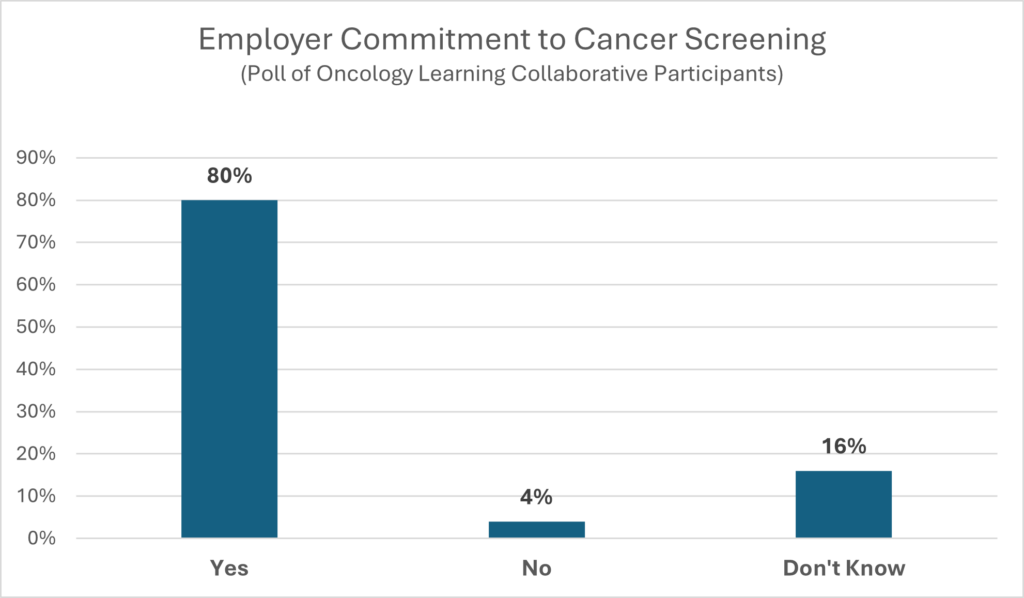
80% of employers who participated in the OLC receive and review data from their health plans on cancer screening rates.
Closing gaps to cancer screening is top of mind for employers. This goes beyond addressing access issues to include ongoing examination of data to uncover employees and employee communities that may not be taking advantage of no- and low-cost screenings.
Dan Dentzer, Manager of Health and Welfare Strategy, United Airlines
“To close screening gaps we rely on effective outreach and communication. UnitedHealthcare uses navigators and other partners.
We’ve looked closely at the safe harbor provision within the IRS regulations and made sure things like dense tissue mammograms and colonoscopy screenings when doctors are removing the polyps during the screening process are paid at 100%. Only when cancer is discovered is it covered at less than 100%. We are also doing beta programs where skin cancer screenings are available on-site. Make sure to consider everything in your environment with these programs; even having a cover to block any access to cameras. In the end, our goal is to remove any barriers.”
Sherri Samuels-Fuerst, VP of Total Rewards, Sargento Foods
“From a prevention standpoint, sometimes it is access. Some of the ways we remove care barriers include bringing in mobile mammography vans, having dermatologists on-site to conduct screenings, and educating about the value of consulting with nurse practitioners. Additionally, healthcare professionals at our on-site health and wellness centers help people review their electronic medical records, and/or their screening or vaccines to make sure they are up to date based on their age and gender.
I have mentioned the on-site mobile mammograms and the resources we use for prevention and education. We also brought dermatologists on-site. These programs fill up very fast and they have diagnosed a few cancers. The mobile mammograms all offer ultrasound for high-density breasts. If we cannot build our own, we work with local oncology and hematology centers. We leverage their nurse navigators and use them to give proactive and preventive education.”
Rosa Novo, Administrative Benefits Director at Miami-Dade County Public Schools
“Cancer represents $78M of our spending and we cover both preventive, diagnostic, and 3-D mammograms at 100%. We also have direct contracts with two local hospitals to provide teachers and school staff with a “Mammography Day” where the hospitals secure all appointments for our staff using a wellness table at the hospital. In addition, we contract with a mobile mammography unit that visits the schools, so our employees don’t need to take time off – and they offer 3-D mammography. We cover both preventive and diagnostic colonoscopies at 100%, and we provide a $100 incentive to when the patient selected a provider with the best quality and cost. We are now at 70% participation for mammogram screenings, 66% for cervical screening, and 37% for colonoscopy. Our average age is 41 and according to available data, our screening results are aligned with other public sector employers.”
Susan McBroom, Director of Human Resources, Patriot Rail Company
“We cover colorectal cancer screening at 100% as preventive and offer a $100 incentive for both the primary care provider and skin screenings if they receive them every year. It has increased the participation rates for both.”
Carole Mendoza, VP of Benefits, Voya Financial
“We receive data on cancer screening rates, and we can sort the data by race, ethnicity, and socioeconomic status. We found that with high social risk comes higher severity, later-stage cancers, and higher costs. These higher-risk employees probably do not have primary care providers. They only go see a physician when a problem arises.”
The American Cancer Society Breast Cancer Awareness Employer Toolkit is a comprehensive resource designed to help organizations educate their workforce about breast cancer, promote early detection, and support employees affected by the disease. This toolkit provides employers with a variety of ready-to-use materials, including fact sheets, digital content, email templates, posters, and event planning guides for Breast Cancer Awareness Month and beyond. It aims to raise awareness of the importance of regular screenings, such as mammograms, and offers guidance on fostering a supportive workplace environment for those undergoing treatment. By using the toolkit, employers can play an active role in reducing the impact of breast cancer through employee engagement, health promotion, and access to credible information and resources.
Cancer Screen Week
Screening for Cancer is Important for your Health
Health systems leverage patient engagement tools to close gaps in cancer screenings
Updated Lung Cancer Screening Guidelines – November 1, 2023 American Cancer Society Press Release
Lung Cancer Screenings: What Employees Should Know
Lung Cancer Screening Patient Guide
The Importance of Screening for Lung Cancer
Lung Cancer Awareness Employer Toolkit 2025
An Employer’s Guide to Prostate Cancer (Pfizer)
Prostate Cancer Awareness Employer Toolkit 2024
Colorectal Cancer Awareness Employer Toolkit 2025
Skin Cancer Awareness Employer Toolkit 2025
When a Spot is More than a Spot – Skin Cancer
Multi-Cancer Early Detection (MCED) Tests
Currently, there is one MCED test available in the market, with about 20 tests in development. These tests are also called liquid biopsies. An advantage of MCED tests is that they require a single blood draw. The currently available MCED test looks at about 70% of cancers for which there is no screening available, while also picking up on cancers for which there are no screenings. These tests can also enable more targeted treatments.
The currently available test is not yet FDA approved and, therefore, not covered by insurance. Out-of- pocket costs are $949 at this time. Some employers have already started to cover the MCED test for certain subpopulations of their plan members (e.g., by age or risk factors). Research trials are underway in the US and in the United Kingdom. Questions to be answered in the research trials include whether the tests are effective in reducing cancer mortality and whether there is potential for overdiagnosis.
As such, there are coverage, access, and equity questions that employers need to consider. Check back here for updates on MCED as these tests are “game-changers.” Study results and FDA approval will be important to consider.
When it comes to diagnosing and treating cancer, the sooner the better. Primary care providers play a significant role in early diagnosis of cancer. One of the most useful questions that can be asked when patients visit their primary care providers is “Have you been having any annoying or concerning issues with your body that have lasted longer than a couple of weeks?”
This one question gives a patient permission to talk about even the little things that they would not otherwise feel comfortable “bothering the doctor with.” This is when things like fatigue, lumps, chronic cough, sores that do not heal, unintentional weight loss or gain, changes in bowel habits, hoarseness, mild pain, night sweats, vision changes, and a multitude of other symptoms of cancer are revealed and can be further investigated. The investigation begins with a complete personal and family medical history and physical examination followed by other diagnostic testing.
Sherri Samuels-Fuerst, VP of Total Rewards, Sargento Foods
“Before a person may be diagnosed, we work with our on-site Health and Wellness Center to promote preventive screenings. They do the scheduling for our employees when we bring in mobile mammography and the dermatology clinic and these appointments fill up quickly. Over the last couple years, we built a partnership with our local oncology and hematology providers to have patients use our Health and Wellness Center in a variety of ways. For example, once an individual is diagnosed, the center is available to draw labs, and this helps them avoid leaving work. The local oncology and hematology providers share the results with the employees’ providers. We have dieticians available to help support nutritional needs as well as have a work-life mentor, which is really an EAP, to support mental well-being throughout diagnosis, treatment, and hopefully through their recovery. We also connect the nurse navigator at the provider’s office with the nurse practitioner at the on-site Health and Wellness Center to provide holistic support. We are working with our PBM and our on-site Health and Wellness Center for site-of-care strategies. Specifically, we are trying to provide fluids at the on-site center as needed and appropriate. We are trying to keep it easy, accessible, and affordable. The patients really trust the on-site Health and Wellness Center because as much as we encourage people to have a primary care provider, they really leverage and use the on-site center. They trust the providers in the center with their health and wellness needs.”
Kenneth Aldridge, Director of Health Services, Rosen Hotels and Resorts
“For our employees, we have traditional strategies such as awareness campaigns to urge associates to get screened and to learn how to be aware of the signs and symptoms of cancer. Onboarding of new associates includes all appropriate screenings at our medical center. We recently brought on mobile dermatology at all locations and found three melanomas in the school district. One was invasive, so we are saving lives. We have been doing mobile mammograms at Rosen Medical Centers since 2007. For colorectal screening, we offer colonoscopies and Cologuard®. We had a 70% return with 9%-10% positive colorectal cancer. We are working with our local specialty lab on other screening options as well. When you look at the specificity and the sensitivity it is equivalent to Cologuard®, but more expensive. From Rosen’s perspective, we would rather pay for that than someone losing their life to colon cancer or undergoing difficult colon cancer treatment.”
© Copyright 2024 Central Florida Health Care Coalition, Incorporated d/b/a Florida Alliance for Healthcare Value
The Central Florida Health Care Coalition, Incorporated d/b/a Florida Alliance for Healthcare Value is providing this information to our employer members solely in our capacity as a 501c3 nonprofit education organization and not as advice in any capacity. The information that is not in the public domain is private and confidential.
