

Oncology Learning Collaborative Partnership
Navigating cancer care and care options have become complex and often overwhelm the patient, family and caregivers:
Diagnostic testing and treatments have expanded but come with pricing and reimbursement challenges.
Variations in oncology care occur across settings and programs, even from provider to provider.
Employees face reimbursement challenges, including increased billing errors.
Inefficiencies drive treatment delays and misdiagnosis.
 The consequences for patients and families can be devastating. Some 40% of cancer patients spend their life savings in the first two years of treatment. Cancer patients were 71% more likely than Americans without the disease to have bills in collections, face tax liens and mortgage foreclosure, or experience other financial setbacks. This leaves no money for palliative or hospice care. Most cancer patients would benefit from mental health support but do not receive it during their treatments/cancer journey.
The consequences for patients and families can be devastating. Some 40% of cancer patients spend their life savings in the first two years of treatment. Cancer patients were 71% more likely than Americans without the disease to have bills in collections, face tax liens and mortgage foreclosure, or experience other financial setbacks. This leaves no money for palliative or hospice care. Most cancer patients would benefit from mental health support but do not receive it during their treatments/cancer journey.
Employers face challenges, too, as they try to understand the social risk factors and mitigate the social needs of the employees. Often, they cannot address the underlying social and economic conditions their employees live in. And while employers want to help, privacy is important – employees like having “anonymous, non-judgmental” support outside of the work setting when dealing with serious health conditions like cancer.
To alleviate the stresses on cancer patients, many benefit plans offer care managers or care navigators. They serve as advocates for the patient and help them access resources as they undergo treatment. Benefit plans offer other support, including mental health, palliative care, and survivorship services. All are further addressed in this section.
Care Managers and Care Navigators
Employers are finding that the most helpful thing they can do is provide care managers and care navigators for plan participants dealing with cancer.
Care managers assess patients’ physical, psychological, and social needs, develop care plans, coordinate services and resources, monitor patient progress, and provide education and support to patients, their families, and caregivers. Care navigators are focused on similar support but often address barriers to care and help manage financial issues. They may look for ways to lower costs or set up payment plans. A navigator may be a nurse navigator or a financial navigator.
The National Patient Advocate Foundation (NPAF) environmental scan in 2020 revealed six domains as key features of providing high-quality needs navigation services. They include:
- Financial advocacy
- Financial care planning
- Medical billing assistance
- Social needs assistance
- Insurance and enrollment advocacy
- Workplace services and support
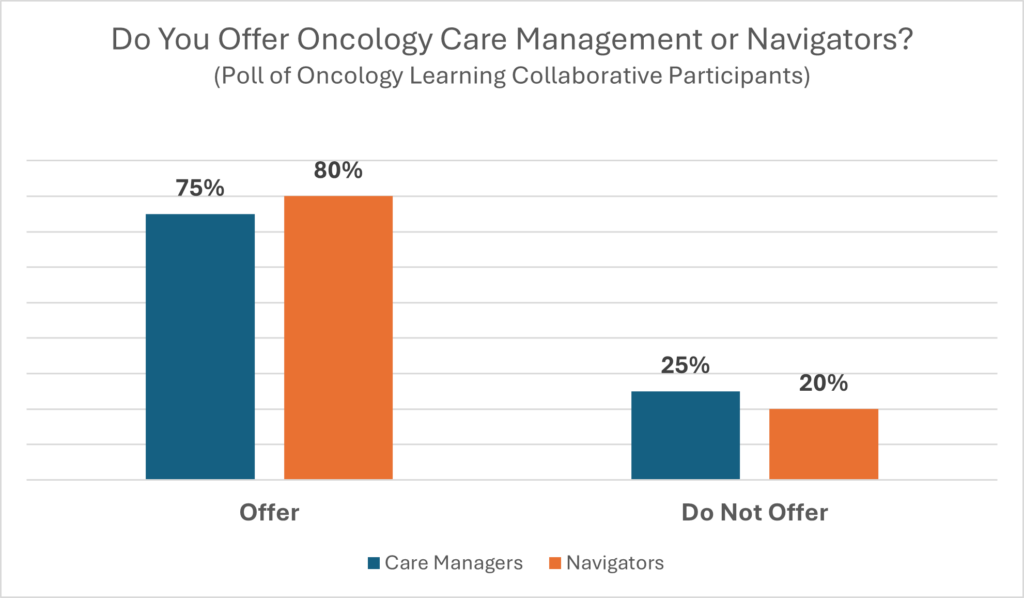
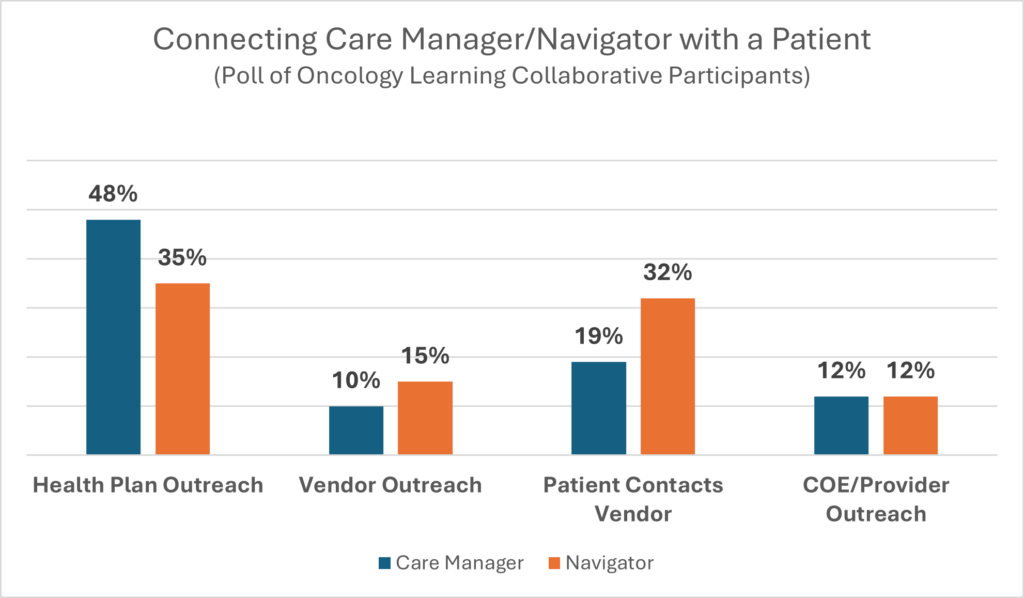
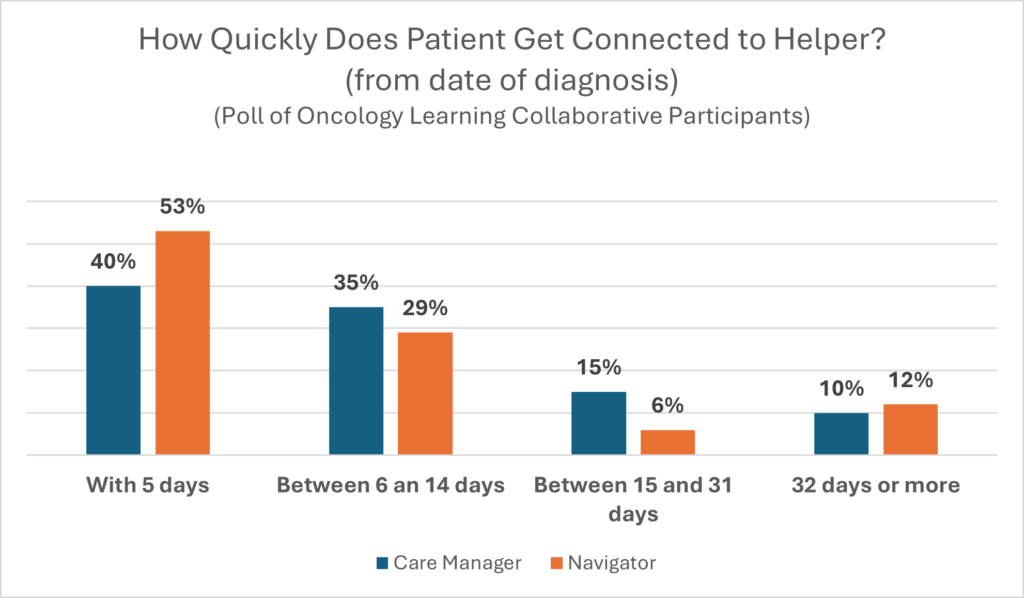
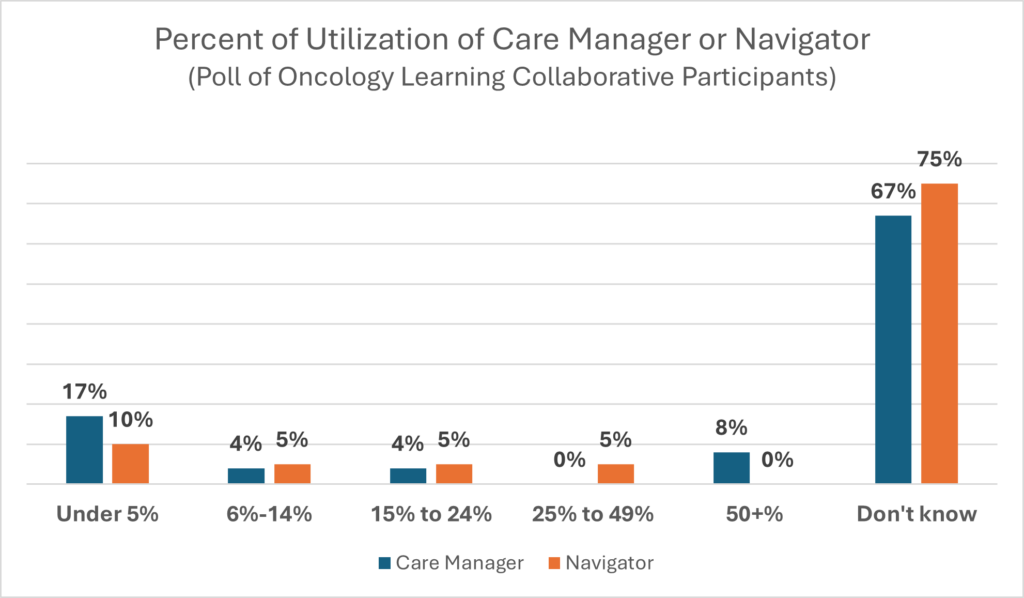
Employers who participated in the Oncology Learning Collaborative were polled on their care manager/navigator experiences. Here are the results.
Lea Ann Biafora, CEO/Founder of Professional Cancer Care Experience Advisors, Beacon Advocates
“MarineMax has oncology social workers who work with Beacon Advocates to help connect patients to psychosocial support. Palliative care is also something we use with every oncology and liver disease case. Most nurse navigators are varied within our healthcare systems so there is no consistency. Since there is a great deal of fragmentation of care in our healthcare system, we serve as the quarterback between all the stakeholders. It is our goal to get the patients connected to providers within their communities, along with the nonprofits in their area. For example, if they have leukemia, we connect them with leukemia support organizations. We also try to stay knowledgeable about innovations so if clinical trials are taking place, we know about them. The goal is to ensure everyone is making informed decisions, recognizing that each individual is different with different backgrounds.”
Rosa Novo, Administrative Benefits Director at Miami-Dade County Public Schools
“We have developed our own in-house cancer support materials since finding some disconnect with what the health plan was sending to members. We also recognize that typically, employees trust the information disseminated by their employers before any other sources. Although we use the information provided by our healthcare carrier, the bulk of it is not in multiple languages so we create everything in English, Spanish, and Haitian Creole. We also provider information on additional resources that include and are not limited to healthy eating and the importance of being active, plus information on disability solutions and mental health support.”
Carole Mendoza, VP of Benefits, Voya Financial
“We offer our employees AccessHope, which provides cancer services and navigation. In 2022, two people used them and one used them for an advisory review, reporting 100% satisfaction. Of course, I don’t believe we only had two cancer patients. Currently, employees or their family members must self-refer so to increase participation, I am working on converting to AccessHope reaching out to cancer patients they identify via a claim feed from the insurance company. A pilot program had very low participation until we did a communication campaign in which we asked if you or anyone you love has cancer. Over 180 people called the first day, which slowly trailed off.”
Dan Dentzer, Manager of Health and Welfare Strategy, United Airlines
“We work with local oncology and hematology centers. We leverage their nurse navigators and use them to give proactive and preventive education.”
Sherri Samuels-Fuerst, VP of Total Rewards, Sargento Foods
“We have both navigators and care managers. Patients get connected once they have a diagnosis. They are in shock about their diagnosis, so we hope the navigation services and case management are working together for them. We don’t have a specific cancer bolt-on or specific services for oncology. We use the general case management of UHC’s UMR which does include an oncology component. We started using Quantum as a single point of contact for navigation services in January, but utilization is fairly low. For those who want it, we also have the local oncology and hematology offices with whom I am working. Their nurse navigators or case managers can be the patient’s sounding board when they don’t understand what they are hearing. I am not sure how to get them connected to the patient because I don’t want our people to think they have to go and that they have to use them because they are one of many options. We do have a way to go when it comes to communicating with employees about the services and getting employees to engage with Quantum. You have to communicate, communicate, and then communicate more while also making sure you don’t cannibalize your other communications. Internally, I am working with our leave coordinator. This person is a centralized point for education, tools, or solutions. It takes multiple efforts, and you have to make each effort multiple times.”
Cancer Navigation Program Pilot
The Florida Alliance and the Patient Advocate Foundation partnered to create an innovative, employer-based benefit program designed to help employees and their dependents more effectively navigate their cancer treatment journey by:
- Providing insightful and proactive benefit education
- Making connections to the social and practical community resources they are eligible for but may not know about
- Providing critical, responsive support for access to care and for financial barriers that impact and impair the ability to access and afford care
 The pilot was conducted with The Walt Disney Company and Orange County Public Schools and funded by Genentech. The goals of the program were to improve employee understanding and utilization of benefits to reduce financial and emotional stress, have a positive impact on employee productivity and satisfaction, and improve access and adherence to care.
The pilot was conducted with The Walt Disney Company and Orange County Public Schools and funded by Genentech. The goals of the program were to improve employee understanding and utilization of benefits to reduce financial and emotional stress, have a positive impact on employee productivity and satisfaction, and improve access and adherence to care.
Serving as a complement to the medical case management programs offered by both the health plan and the provider, the cancer navigators were trained professionals and trusted resources who had the intent of helping patients overcome physical, emotional, social, and financial barriers to receiving timely cancer treatment. The cancer navigators provided support in the following areas:
- Proactive benefit education, navigation, and empowerment
- Community resource navigation and enrollment
- Benefit utilization navigation and intervention
- Responsive intervention and solutions for specific access to care and financial issues faced by the cancer patient and their family
This pilot program was provided as an offering by the employer to eligible plan members. To be eligible for the program, the individual had to be enrolled in the employer-sponsored group health insurance plan as an employee, spouse, or dependent and had to have a diagnosis of cancer. The program was sponsored by the employer and all the services were provided to the employee free of charge. The employer paid $200 per participant.
Individuals accessing the program were assigned a personal cancer navigator who provided education, navigation, and hands-on interventions throughout the cancer experience. There was no limit on the number of times assistance could be requested from the cancer navigator.
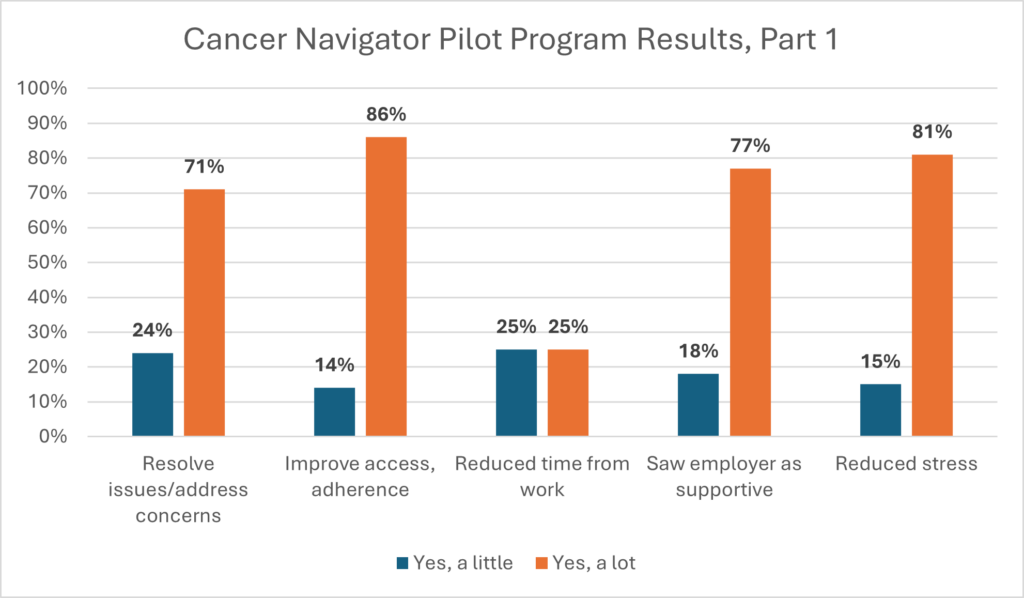
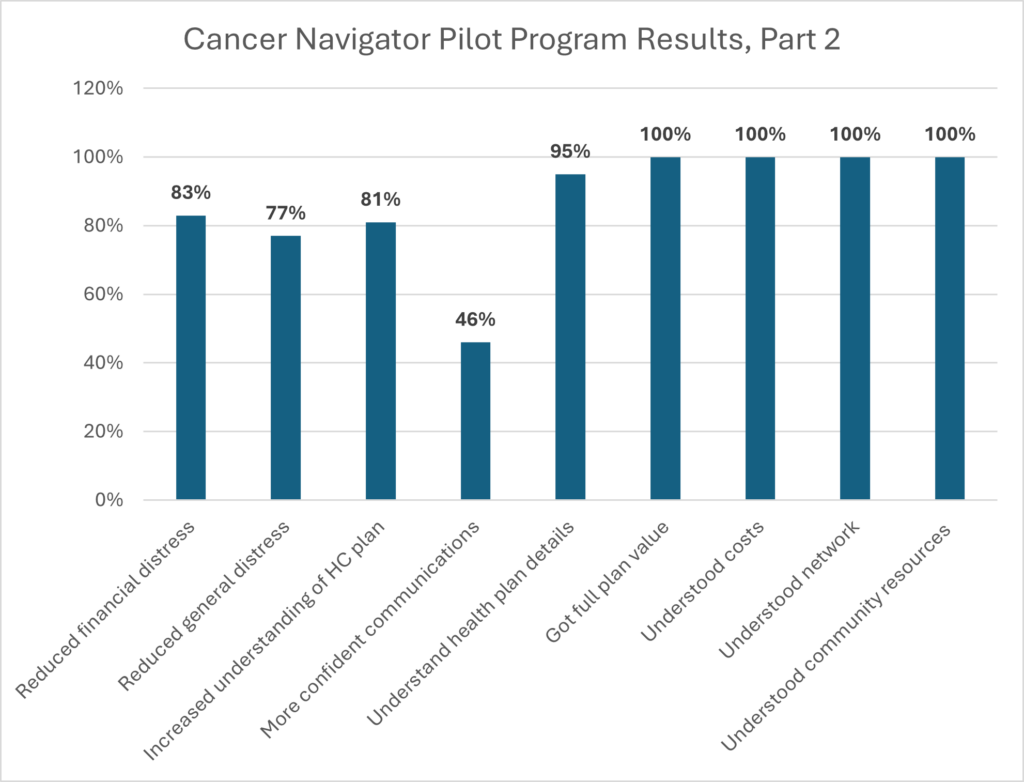
Results are shown in the chart below.
Carole Mendoza, VP of Benefits, Voya Financial
“Providing cancer support is a safety net for our employees. One of the components of our cancer support is where someone with a new diagnosis can call in, get questions answered, and learn what the journey is going to be. Another component is access to two expert advisors: 1) the employee or family member can call in for an expert or second opinion and our vendor partner, AccessHope, coordinates with the local oncologist to make sure the diagnosis and treatment recommendations are correct, and 2) An expert advisory component called Accountable Precision Oncology automatically reviews claims data and does an external review for us. Although our utilization isn’t huge, they are making more outbound calls. And, even though it has been more of a pull from employees, those who have used it have loved it because you don’t want to be alone when you have a cancer diagnosis. It is helpful to have an expert to rely on that you and your family can use for help navigating the very difficult situation.”
Sherri Samuels-Fuerst, VP of Total Rewards, Sargento Foods
“We are implementing a care navigation service for all the healthcare needs of our population starting in 2024 using the care navigator at the local oncology-hematology offices. The service is aware of our on-site Health and Wellness Center and they will help coordinate care, direct employees and their families to resources, and make the healthcare journey easy, accessible, and affordable. We will also collaborate and work together on educating our employees on certain things, so they are not inundated with multiple pieces on the same subject from different vendor partners. Using vendor summits to assure that all vendors understand the types of benefits and cancer-related services we offer helps assure that when they are contacted, they may educate on the services the employee or family member did not know were available, and that they also can do a soft transfer.”
MarineMax Case Study
MarineMax contracted with a partner who employs nurse-led cancer care management and offers a unique end-to-end solution that focuses on early detection all the way to return-to-work or end-of-life.
Roles and Communications
The vendor’s oncology nurse case managers have over 10 years of oncology experience and are patient advocates who go through the entire patient journey. They use flyers, postcards, a dedicated web page, and quarterly newsletters to communicate with the employees and their family members. They are also increasingly using testimonials.
Program Elements and Activities
Their customizable cancer care guidance programming:
- Focuses on risk assessments to be more proactive.
- Reaches the patient earlier by using triage data, human resource professionals, employee self-referrals, and teammate referrals.
- Eliminates waste by making sure documents are moving between the interested parties.
- Makes sure the right diagnostic tests are completed and that the treatment plan is right for the patient.
- Shares the decision-making with the patient and the providers.
- Reviews the clinical treatments, gets second opinions, reviews cases, and has geneticists review cases.
- Becomes the liaison between the different stakeholders and collaborates with the medical team.
- Uses safe, trusted advisors.
- Gives the patient, families, and caregivers tools and access to financial resources and care.
- Guides them through working with cancer and helps them understand their EAP, short- and long-term disability (STD LTD), and other benefits as well as helps guide them through side effects.
- Places importance on surveillance and survivorship.
- Coordinates, if necessary, the end-of-life process. They have this discussion with everyone from stage 0 to stage 4.
- Reviews clinical trials for appropriateness.
Results
- Expedited right care at the right time in the right place. Ensures the patient is using the right benefit like STD or LTD.
- Reduces emergency department visits and unnecessary or duplicate tests.
- Improves productivity.
- Earlier and appropriate transition off-plan.
- Less costly end-of-life care.
- Increased clinical trial utilization.
- Bridges communication gaps.
- Empowers employees and gives them a better cancer experience with better outcomes.
- Helps remove barriers to care.
Contributed by Ray L. Bowman, PhD., Retired Senior Vice President, Talent and Team Development, MarineMax.
Psychosocial Support
Psychosocial support ensures that patients receive needed mental health support throughout the cancer journey.
Hospice and Palliative Care
As a newer type of care that takes people’s individual needs into account, palliative care aims to meet their medical, physical, spiritual, and emotional needs. Its main goal is to help relieve mental and physical symptoms that result from cancer or treatments, including the immense stress experienced by patients and their caregivers.
Although the objective of hospice and palliative care is pain and symptom relief, the prognosis and goals of care tend to be different. Palliative and hospice care are similar in terms of the services provided; palliative care is provided to those receiving ongoing treatment for cancer, while hospice care is intended for terminally ill patients who have stopped treatment and typically have been deemed by a physician to have six months or less to live. Both types of care are provided by special teams of professionals that may include physicians, nurses, social workers, therapists, psychologists, and clergy members.
The Center to Advance Palliative Care (CAPC) and the National Hospice and Palliative Care Organization (MHPCO) provide directories to assist in locating palliative caregivers. Employers should ensure that palliative care is a covered benefit (as it is not always covered), and their members receive just-in-time communications and assistance in accessing this important benefit via case managers/navigators.
Catalyst for Payment Reform provides a comprehensive toolkit for employers to develop a new palliative care strategy or infuse palliative care into existing healthcare programs.
Coverage for hospice services is 100% by Medicare, Medicaid, and private insurance, but in many cases the patient has to give up curative treatment to access hospice services. Palliative care reimbursement varies by insurance plan. Most money on cancer care is spent in the last two weeks of life, but it is not on palliative or hospice care, which often is more efficient, supportive, and less expensive.;
Lea Ann Biafora, CEO/Founder of Professional Cancer Care Experience Advisors, Beacon Advocates
“I would like to reiterate the importance of palliative care to help with symptom management and I want to remind everyone not all systems or community services offer it.”
© Copyright 2024 Central Florida Health Care Coalition, Incorporated d/b/a Florida Alliance for Healthcare Value
The Central Florida Health Care Coalition, Incorporated d/b/a Florida Alliance for Healthcare Value is providing this information to our employer members solely in our capacity as a 501c3 nonprofit education organization and not as advice in any capacity. The information that is not in the public domain is private and confidential.
